Ankle arthroplasty – A review and summary of results from joint registries and recent studies (Bone and Joint UK)
-
Total ankle arthroplasty offers a reasonable alternative to ankle arthrodesis in carefully selected patients.
-
It is debatable whether rheumatoid arthritis patients have better outcomes compared with those who have ankle arthroplasty for either primary osteoarthritis or post-traumatic arthritis.
-
Aseptic loosening and infection are the most common complications requiring revision.
-
It is worth noting that some of the best survival rates are seen in the surgeon-designer case series.
-
The uncemented mobile or fixed bearing prostheses have better outcomes compared with their older counterparts.
-
There is no convincing evidence to suggest superiority of one design over another among the currently available prostheses.
-
Ankle arthroplasty surgery has a steep learning curve; the prosthesis choice should be driven by the surgeon’s training and experience.
Introduction
Ankle fusion has traditionally been the “gold standard” treatment for end-stage ankle arthritis. However, because of recent improvements in prosthetic design and encouraging short- to medium-term results, there has been a renewed interest in total ankle arthroplasty.1 In this article, we look at recent outcomes derived from various joint registries and research papers to discuss the current indications, trends and survival of ankle arthroplasty.
Search methodology
Information was obtained by checking the official websites of various joint registries or published studies derived from joint registry data. The second set of references were obtained by performing a PubMed search for articles with the keywords “total ankle replacement”, “total ankle arthroplasty” and the brand names of the most commonly used ankle arthroplasty prostheses. When there were different studies describing follow-up of the same cohort, then the later study with longer follow-up was chosen. If a systematic review of a particular brand of ankle prosthesis was discussed, then to avoid duplication, individual studies from that systematic review were not discussed.
Indications and prosthesis types
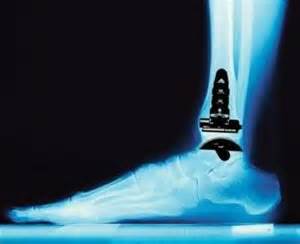
In contrast to hip and knee joints, the ankle joint is less commonly affected by primary arthritis.2 Post-traumatic arthritis is the most common occurrence.3,4 Ankle arthroplasty, when compared with fusion, has an added advantage of maintaining joint movement, besides the primary goal of providing pain relief. The first-generation prostheses were non-modular and made up of all-polyethylene tibial components with a metallic Talar component fixed with bone cement. The newer generation prostheses are cementless, metallic and coated (hydroxyapatite or porous), with intervening polyethylene, which can either be fixed or mobile.5
The ideal patient for ankle arthroplasty has been described as a “middle-aged or elderly patient with an anatomically aligned ankle and heel, whose ankle has relatively preserved range of movement that includes at least 5 degrees of dorsiflexion”.6 Thus, ankle arthroplasty is not an option for every patient needing a fusion. Optimal outcomes can be achieved by identifying those subsets of patients with arthritis who meet the criteria (Figs 1and 2).


The most commonly used second-generation prostheses are (arranged alphabetically):
-
Agility (DePuy, Warsaw, Indiana)
-
Buechel-Pappas (Endotec, South Orange, New Jersey)
-
Hintegra (Newdeal SA, Lyon, France)
-
Mobility (DePuy – discontinued)
-
Salto Talaris Total Ankle Prosthesis (Tornier, Stafford, Texas)
-
Scandinavian Total Ankle Replacement (STAR) prosthesis (Waldemar Link, Hamburg, Germany).
Review of joint registry data
The Australian Orthopaedic Association, in their supplementary report, looked at all ankle arthroplasties between July 2006 and December 2016.7 There was a total of 2235 ankle arthroplasties (39% female and 61% male patients) (Table 1). The most common age group was 65 years to 74 years (median 66 years). Osteoarthritis (92.8%) was the most common indication for ankle arthroplasty, followed by rheumatoid arthritis (5.5%). The Salto Talaris was the most commonly used prosthesis for ankle arthroplasty. The cumulative percentage revision at five years was 4.6% when rheumatoid arthritis was the primary diagnosis, in contrast to a cumulative percentage revision of 10.2% in cases of osteoarthritis. Thus, the data from the Australian joint registry supports the view that patients with rheumatoid arthritis have significantly lower revision rates compared with those with osteoarthritis. The most common indication for revision was loosening/bone lysis (in 29.2% cases). The data from Australian joint registry had the second largest sample size of the reports considered.
| Source | Time range | Total cases | Most common indication | Most common prosthesis overall | Most common prosthesis in latest year | Revision rate |
|---|---|---|---|---|---|---|
| Australian Orthopaedic Association supplementary report | 2006 to 2016 | 2235 | Osteoarthritis (92.8%) | Salto Talaris | Salto Talaris | 4.6% (rheumatoid arthritis); 10.2% (osteoarthritis) at 5 yrs |
| Finnish Arthroplasty Register | 1982 to 2006 | 573 | Rheumatoid arthritis (49%) | AES | – | 17% at 5 yrs |
| UK National Joint Registry | 2010 to 2016 | 3899 | – | Mobility | Infinity | 7.7% at 5 yrs |
| New Zealand Joint Registry | 2000 to 2016 | 1380 | Osteoarthritis (75.07%) | Salto Talaris | Salto Talaris | 18.4% at 10 yrs |
| Norwegian Arthroplasty Register | 1994 to 2015 | 1047 | Post-traumatic osteoarthritis | Link STAR | Salto Talaris | – |
| Swedish Ankle Register | 1993 to 2010 | 780 | Rheumatoid arthritis (36%) | Link STAR | Rebalance | 31% at 10 yrs |
Skytta et al8 based their study on ankle arthroplasties registered on the Finnish Arthroplasty Register between 1982 and 2006. There was a total of 573 ankle arthroplasties performed, and they restricted their analysis to prostheses series with a minimum of 40 reported cases. Only two prostheses, the Link STAR and Biomet AES (Ankle Evolutive System), met this inclusion criterion, constituting a sample size of 515 (298 AES and 217 Link STAR). The survivorship was 83% at five years, and there was no statistically significant difference based on age, disease subgroup, gender or prosthesis used. The authors excluded prostheses with low volumes which can account for various other variables that potentially affect survivorship. They went on to recommend that total ankle arthroplasty only be performed at specialist centres, and surgeons doing those procedures should operate on or assist at least 25 cases annually. Although their analysis of the registry did not show a difference in revision rate between low- and high-volume hospitals, they made these recommendations based on previous studies looking at ankle, shoulder and hip arthroplasty. It was not clear how the figure of the “25 cases per surgeon annually” was reached.
In their annual report, the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man (NJR) included a total of 3899 primary ankle arthroplasties performed between 2010 and 2016.9 The median age at surgery was 68 years and the Mobility prosthesis (28.9% of all ankle arthroplasties) was the most commonly used prosthesis until it was withdrawn from the market in June 2014. A Kaplan-Meier estimate showed a cumulative probability of revision of 7.7% at six years, with aseptic loosening as the most common cause of revision. It is pertinent to note that under-reporting of ankle revision has been identified as an issue, hence the conclusions drawn from survival analysis are not entirely reliable.
The New Zealand Joint Registry reported a total of 1380 cases (842 male, 538 female patients) over 17 years with a mean subject age of 65.91 years.10 Osteoarthritis was the most common indication for ankle arthroplasty (75.07%). Loosening of either the tibial or the talar component was the most common cause for revision. In this registry, for the last five years (2012 to 2016), the Salto Talaris implant was not only the most used prosthesis, but also had the lowest revision rate. Kaplan-Meier survival analysis of all the ankle arthroplasties on the New Zealand Joint Registry showed a revision rate of 18.4% at ten years.
The Norwegian Arthroplasty Register reported a total of 1371 ankle arthroplasties (1047 primary and 324 revision) from 1994 to 2015.11 The percentage of revision ankle arthroplasties remained in the range of 28% to 35% from 2011 to 2015. The Link STAR remained the most common prosthesis used until 2013, after which Salto Talaris took the top spot for the final two years of the report. Although there is year to year variability, overall, post-traumatic osteoarthritis was the most common indication for ankle arthroplasty. The report did not comment on prosthesis survival rates.
Henricson et al12 analyzed the Swedish Ankle Register to look for ten-year survival. Between April 1993 and June 2010 a total of 780 primary ankle arthroplasties were reported. The most common indication was rheumatoid arthritis (36%), followed by post-traumatic arthritis (34%), primary osteoarthritis (24%) and others (6%). The overall survival was 81% at five years, falling to 69% at ten years. Aseptic loosening was the most common indication for revision. The single-coated Link STAR prosthesis had a statistically significant higher revision rate compared with other prostheses.
With regard to the number of ankle arthroplasties performed, joint registry data show an initial slow and steady increase followed by recent plateauing (Fig. 3). The Australian registry even shows a downwards trend.

Review of recent prosthesis-specific studies
In a systematic review of 14 studies dealing with the Agility total ankle arthroplasty, it was found that revision rate was 9.7% at a mean follow-up of 22.6 months (Table 2).13 In all, 81.3% of these revisions involved component arthroplasty, 15.2% arthrodesis and 3.6% required amputation. Sub-classification of the studies into inventor and non-inventor groups yielded revision rates of 6.6% and 12.2% respectively. Of the 14 studies included, 12 were level IV or level V evidence. This highlights the lack of higher level data for this prosthesis. However, our review showed that most studies involving ankle arthroplasty are of level IV or V evidence. Roukis13 did well to include studies in the French and German literature using computer-based translation software. Another important feature of this review was that no study was excluded because of inability to obtain the paper, making it a comprehensive review on this prosthesis. Another recent independent case series looking at 107 Agility ankle arthroplasties with a mean follow-up of 9.1 years showed a survival rate approaching 80% at nine years.14
| Serial no | Author | Type of study | Prosthesis | Sample size | Survival |
|---|---|---|---|---|---|
| 1 | Roukis 201213 | Systematic review | Agility | 2312 | 90.3% at 22.6 mths |
| 2 | Raikin et al 201714 | Case series | Agility | 107 | 80% at 9 yrs |
| 3 | Buechel et al 200315 | Case series | Buechel-Pappas | 50 | 93.5% at 10 yrs |
| 4 | Giovanni et al 200616 | Case series | Buechel-Pappas | 31 | 93% at 8.3 yrs |
| 5 | Barg et al 201317 | Case series | Hintegra | 684 | 84% at 10 yrs |
| 6 | Choi et al 201318 | Comparative case series | Hintegra | 32 | 87.5% at 53 mths |
| Mobility | 35 | 97.1% at 34 mths | |||
| 7 | Wood et al 201019 | Case series | Mobility | 100 | 93.6% at 4 yrs |
| 8 | Muir et al 201320 | Case series | Mobility | 125 | 94.4% at 4 yrs |
| 9 | Bonnin et al 201121 | Case series | Salto | 85 | 85% at 10 yrs |
| 10 | Schweitzer et al 201322 | Case series | Salto Talaris | 67 | 96% at 2.8 yrs |
| 11 | Brunner et al 201325 | Case series | Link STAR (uncemented) | 77 | 70.7% at 10 yrs |
| 12 | Zhao et al 201126 | Meta-analysis | Link STAR (uncemented) | 2088 | 71.1% at 10 yrs |
A prospective study of 50 ankle arthroplasties carried out by the inventors of the Buechel-Pappas ankle arthroplasty resulted in 88% excellent to good clinical outcomes at a mean follow-up of five years.15 Survival analysis demonstrated a survival of 93.5% at the end of ten years.
Giovanni et al16 reported a prospective study using the Buechel-Pappas ankle arthroplasty prosthesis exclusively in 31 patients with rheumatoid ankles. This showed a survivorship of 93% at 8.3 years. Of the 28 ankles available for follow-up, 96% reported no pain. The authors went on to recommend ankle arthroplasty as a good alternative to fusion in patients with rheumatoid arthritis. According to them, a good outcome is attributable to the fact that patients with advanced rheumatoid arthritis and multiple joint involvement have low functional demand, making them ideal candidates for total ankle arthroplasty. In this study, there was a high incidence (32%) of intra-operative medial malleolar fractures. Since there were no age-matched controls without rheumatoid arthritis, it was not possible to conclude whether this complication is related to prosthesis design/technique or poor bone quality seen in rheumatoid patients.
Barg et al17 carried out a retrospective review of collected data for survivorship of Hintegra ankle arthroplasties performed in 722 ankles; they found it to be 94% at five years and 84% at ten years. Since the study included three different generations of the prosthesis, the authors not only compared one generation with another but also looked for independent risk factors for prosthesis failure. In their regression analysis, they found that age less than 70 years, primary/post-traumatic arthritis and the use of an older generation prosthesis (first and second) were independent risk factors for prosthesis failure.
In their retrospective comparative study between Mobility and Hintegra ankle arthroplasties, Choi et al18 found no significant difference in clinical outcomes. However, heterotopic ossification was much more common with Hintegra implants, and intra-operative medial malleolus fracture was seen commonly with the Mobility ankle arthroplasty. The study has drawbacks of a small sample size (32 Hintegra and 35 Mobility), short follow-up (mean 34 months) and the fact that it is retrospective in nature.
In a case series of 100 Mobility total ankle arthroplasties, the four-year survival was 93.6%.19In all, 97% of patients were satisfied or very satisfied with their ankle arthroplasties. Taking into account the prosthesis survival and clinical outcomes this is one of the best results. However, it is to be noted that this is a single surgeon series with the operating surgeon-designer having experience of performing more than 400 such procedures.
Muir et al20 reported a retrospective analysis of 129 Mobility ankle arthroplasties with a mean follow-up of 48 months. Rheumatoid arthritis was the indication for surgery in only 12% of the sample. In all, 14% of subjects had a poor outcome based on their pain scores, with a preoperative diagnosis of post-traumatic arthritis being a significant risk factor. The revision rate was 5.6% at a mean follow-up of four years.
Another surgeon-designer series using the Salto Talaris total ankle arthroplasty system reported a survival of 85% at ten years when component revision or fusion was used as the end-point.21 However, if re-operation rate is used as the end-point, the survival at ten years falls to 65%. The study looked at 98 ankles in 96 patients. However, 11 patients (nine dead and two others) were excluded. This left 85 subjects with a mean follow-up of 8.5 years.
The Salto Talaris is a fixed bearing variant of the Salto total arthroplasty system, which is mobile bearing. A study using the Salto Talaris prosthesis involving 67 patients found survivorship of 96% at a mean follow-up of 2.8 years.22 The authors went further to elaborate on the patients’ characteristics including body mass index, smoking status and diabetes. Deep deltoid release (21 cases) was the most common concurrently performed procedure, whereas ankle impingement (six patients) was the most common reason for re-operation. A more recent study using the Salto Talaris implant was a single-surgeon case series of 72 cases with a survival of 97.5% at mean follow-up of 5.2 years.23 The most common indication was osteoarthritis and the most common concomitant procedure was the removal of metalwork.
Kofoed,24 in his prospective study, used the Link STAR prosthesis in 58 ankles (33 cemented and 25 uncemented). There was no loss to follow-up. Survival analysis showed a 12-year survival of 95.4% in the uncemented group compared with 70% in the cemented group. This strongly suggests a better outcome for the uncemented prosthesis over its cemented counterpart. Although this was a prospective case series it does not indicate whether other confounding factors such as age and primary pathology were comparable in both groups.
A recently published prospective observational study of 77 ankles is the longest follow-up (mean 12.4 years) available for the uncemented single-coated Link STAR prosthesis.25 The prosthesis survival was 70.7% at ten years and 45.6% at 14 years. The study is remarkable not only because of the duration of follow-up but also because only two patients were lost to follow-up. Zhao et al26 sum up the results of the Link STAR prosthesis in their meta-analyses of 14 studies amounting to 2088 cases. The survival rates in this review were 85.9% at five years and 71.1% at ten years.
Lefrancois et al27 in their prospective non-inventor series using four different ankle arthroplasty prostheses (Hintegra, Agility, Mobility and Link STAR) achieved comparable outcomes and prosthesis survival with three out of the four prostheses. Mobility had inferior patient-reported outcomes with higher odds of revision.
There are studies which looked specifically at total ankle arthroplasties in rheumatoid patients. Some of the earliest studies reported on first generation cemented prostheses, which had poor outcomes with clinical and radiological loosening at follow-up.28–31 None of these prostheses are in use today.
Kofoed and Sørensen32 in their prospective study using cemented prosthesis reported no significant difference in prosthesis survival between the rheumatoid and osteoarthritis group. Anderson et al33 in their retrospective analysis of an uncemented prosthesis found no significant difference in post-operative scores of patient groups with rheumatoid arthritis, osteoarthritis and post-traumatic arthritis.
Doets et al34 exclusively studied uncemented mobile bearing ankle arthroplasties in 93 rheumatoid patients and reported 84% survival at eight years, with aseptic loosening and persistent deformity as the most important modes of failure. They used the LCS (Low Contract Stress mobile bearing prosthesis) in an initial 19 cases, followed by the Buechel-Pappas design for the remainder. On the contrary, Van Der Heidi et al35 found infection to be the most important cause of failure in their case series of 53 ankle arthroplasties in rheumatoid arthritis, with a mean follow-up of 2.7 years.
Conclusions
In summary, the registry data show big variations in total ankle arthroplasty survival rates. In most registries aseptic loosening is the most common indication for revision. The advantage of using registry data is that it provides large sample sizes to help identify trends. The limitations of registry data are issues with the quality of data, which also includes possible under-reporting of primary/revision cases or misreporting of indications for primary/revision surgery. There is also lag before registry data becomes available, meaning that there is a delay in data showing catastrophic failures of a particular prosthesis. The lack of patient-reported outcome measures or radiological outcomes in registry data is another major disadvantage.
The NJR has the highest number of ankle arthroplasties recorded. The data for total ankle arthroplasty were only added to the registry in 2008. Considering the relatively large numbers it will be interesting to see the outcome data from the NJR in coming years, assuming that the problem of under-reporting of revision procedures is addressed. It is debatable whether rheumatoid arthritis patients have better outcomes compared with those who have ankle arthroplasty for either primary osteoarthritis or post-traumatic arthritis. The studies that show better outcome in rheumatoid arthritis patients attribute it to the fact that these patients have lower functional demands. There is a 10% to 15% possibility of revision by the end of five years and 20% to 30% by the end of ten years. Most studies looked at the revision of prostheses or arthrodesis as the end-point while calculating survival rates. However, if the re-operation rate is considered as the end-point for failure, then the survival rates of ankle arthroplasty decrease further. Aseptic loosening and infection are the most common complications requiring revision. Persistent medial ankle pain is another problem that can compromise clinical outcomes. It is worth noting that some of the best survival rates were seen in the surgeon-designer case series.15,19,24
There is evidence that uncemented mobile or fixed bearing prostheses have better outcomes compared with their older counterparts; however, there is no convincing evidence to recommend one design over another among the currently available prostheses. There is a constant push from manufacturers to develop better prostheses in order to improve survival and produce outcomes comparable with hip and knee arthroplasty. As work continues on that front, it will be useful to look at other patient characteristics such as body mass index, smoking status, medical co-morbidities and other variables, which can help in patient selection and improve implant survival. Since ankle arthroplasty surgery has a steep learning curve, the prosthesis choice should be driven by a surgeon’s familiarity with prostheses and the availability of these.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Funding statement No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.